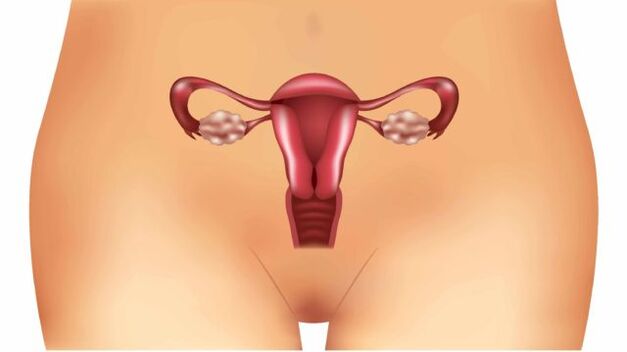
Almost everyone has heard of varicose veins. In most people, this vascular disease is associated with leg problems, but quite often the pelvic organs become the place of localization of the pathological process. One of the types of this pathology is varicose veins of the uterus.
The disease is diagnosed mainly among women or girls who have entered reproductive age, but in some cases it also develops in adolescent girls. To cope with the pathology, it is important to know the main causes and symptoms of its occurrence, as well as to have an idea about the methods of treatment.
Features of the pathology
Varicose veins of the uterus, what is it? This medical term refers to a disease caused by a number of pathological factors affecting the venous network of the pelvic organs:
- Thinning of the vascular walls.
- The formation of vascular nodules.
- Expansion of the venous lumen.
These three factors negatively affect the process of blood circulation in a separate part of the organ and lead to valvular insufficiency of the veins in the same area. The disease is difficult to diagnose due to the lack of obvious clinical signs, and also due to the similarity with diseases of the pelvic organs of an inflammatory nature. For these reasons, pathology is often detected at severe stages, when its treatment is much more complicated.
Gynecologists distinguish two subspecies of the pathological process:
- Varicose veins of the uterus.
- Varicose veins of the cervix.
In any case, the disease is dangerous for its complications, among which there are inflammatory processes covering the uterus, ovaries, and vagina. The most severe complication is infertility.
Causes of the disease
Understanding the underlying factors in the development of the disease provides several key benefits. Firstly, it allows the doctor to diagnose faster and with higher accuracy, as well as prescribe adequate treatment. Secondly, a woman will be able to try to prevent the development of pathology.
Consider the most likely causes of uterine varicose veins:
- Pregnancy is considered the main factor in the development of the pathological process. Already at the embryonic stage, and then as the fetus grows and develops, uterine circulation increases (much depends on the period). At the same time, in vessels with a weakened venous wall, valve function is disturbed, and they are stretched. In addition, a growing fetus increases the load on the pelvic organs, which can also give impetus to the development of the disease.
- Taking hormonal drugs for a long time. Specific drugs adversely affect the condition of the vessels, their walls lose their elasticity.
- Another factor that provokes the disease is reduced motor activity. A sedentary or sedentary lifestyle leads to a decrease in the contractile function of the muscles, the consequence will be a violation of blood circulation.
- Increased physical activity on the pelvic region. In this case, as in pregnancy, blood flow to the pelvic organs, in particular, to the uterus, increases.
- Increased constipation - in this case, the cause of varicose veins again becomes an increase in blood flow. However, the circulation is now increased due to increased intra-abdominal pressure.
- Congenital anomalies in the structure of the uterus.
- Artificial termination of pregnancy.
- Difficult childbirth.
- Inflammatory processes in the pelvic organs.
Symptoms and Diagnosis
The difficulty in diagnosing uterine varicose veins lies in the fact that the symptoms of this disease are disguised as other pathologies. In addition, the clinical picture indicating the development of the disease is rather poor:
- Frequent, recurring more than 3-4 times a week pain in the lower abdomen, closer to the pubic region. The pain syndrome is pronounced, the nature of the pain is pulling and aching. In some cases, the pain is so intense that the woman loses her ability to work, it's hard to even get out of bed.
- More than 80% of women with uterine varicose veins experience discomfort or even pain during intercourse or after it.
- Violation of the menstrual cycle, delays in menstruation up to 50-60 days are possible. In this case, the discharge is often meager, menstruation is stretched in duration over 5-7 days. The prolonged absence of menstruation by many women is taken as the first signs of menopause.
This clinical picture is inherent in a number of other gynecological diseases. For this reason, it is impossible to make a diagnosis only on the basis of symptoms, the doctor is obliged to prescribe a number of diagnostic measures. In addition, in varicose veins of the cervix, the symptoms are about the same.
Important: Varicose veins of the uterus are diagnosed mainly in the second stage, since it is at this time that the described symptoms begin to disturb the woman. The sooner the pathology is detected and its treatment is started, the lower the likelihood of complications, in particular, infertility.
As for directly assigned studies, they are as follows:
- Ultrasound, which is performed by the transvaginal method.
- CT of the pelvic organs.
- Dopplerography.
- Selective ovaricography.
The need for each diagnostic method depends on the data obtained as a result of ultrasound, since it is carried out first.
Features of the disease during pregnancy
Due to the increased load on the body as a whole and the pelvic organs, during pregnancy, the chance of developing uterine varicose veins increases. Until a woman gives birth, the disease is not treatable.

Pathology that develops during pregnancy affects the choice of method of delivery. Very often, the doctor decides to perform a caesarean section. This is done in order to avoid complications in the form of thrombophlebitis, internal bleeding, thrombosis, etc.
Regardless of during what period of pregnancy the disease was detected, a woman needs to be constantly monitored by a doctor in order to monitor the condition of the fetus and the progression of varicose veins.
Important: When planning a pregnancy, undergo an examination to identify uterine varicose veins and other gynecological problems. This will help to avoid complications during childbirth and reduce the risk of fetal developmental pathologies.
Treatment of the disease
To receive qualified assistance with varicose veins, you need to contact a doctor, initially a gynecologist, who will then refer you to a phlebologist.
The basis of treatment is drug therapy, which consists of taking the following medicines:
- Venotonics - drugs of this group have a beneficial effect on the state of blood vessels. They tone the capillaries and blood vessels, reduce their permeability, increase elasticity and strengthen the walls of the veins.
- Drugs to reduce blood viscosity - contribute to a general improvement in the inflow and outflow of blood in the affected vessels, reduce the likelihood of thrombosis. Means of this group are contraindicated in pathologies of the cardiac system.
Important: Any medicine is prescribed only by a doctor, based on preliminary diagnosis, the patient's medical history and taking into account the stage of development of the disease. It is important to observe special care for women in position.
Treatment methods
In addition to drug therapy for a complete treatment, an integrated approach and the implementation of the following recommendations are important:
- compliance with the sleep regimen;
- minimizing physical activity, but at the same time maintaining mobility;
- following a diet that includes a lot of vegetables, fruits, and oils rich in vitamin E;
- supportive sports, therapeutic gymnastics;
- complete exclusion of any bad habits;
- some doctors recommend doing Kegel exercises, which help strengthen the vaginal muscles.
Surgical intervention
Such drastic measures are required in cases where conservative treatment has not brought proper results or the disease has been detected at a late stage. The following methods of surgical intervention are most popular:
- Phlebectomy is the removal of individual sections of small vessels.
- Laser coagulation is the most sparing type of restoration of normal blood flow.
- Sclerotherapy is the introduction into the cavity of a vein of an agent that promotes its gluing. The lack of blood supply in the vessel will lead to its spontaneous elimination.
- In the most severe cases, it is necessary to carry out a complete removal of the uterus, sometimes along with the appendages.
ethnoscience
Alternative methods are one of the options for complex treatment in a conservative way. They are not able to fully replace drug therapy, but can affect the success of therapy in general.
The most effective means of traditional medicine are:
- Infusion of horse chestnut: take 100 grams of chestnut fruit, chop them together with the peel. Pour the resulting raw material with such an amount of vodka that it covers the crushed fruits by 4-5 millimeters. Insist in a dark place for 14-15 days. After that, the infusion is taken 10 drops twice a day. The tool strengthens the vascular walls and thins the blood.
- Lilac tincture: for 0. 5 liters of vodka, you need to take 100 grams of lilac flowers and 30 grams of propolis. All ingredients are poured with vodka and left in a dark place for 30 days (every 2-3 days you need to shake). Then the tincture is filtered and consumed 15 milliliters three times a day before meals.
Remember, before using even the most harmless traditional medicine, you should consult a doctor.
Complications of the disease
Varicose veins of the uterus are dangerous for their complications in the absence of adequate treatment. These complications are as follows:
- internal bleeding;
- thrombosis;
- inflammatory processes of the genital organs;
- menstrual irregularities;
- hormonal dysfunction of the ovaries;
- infertility.
Preventive measures
It is always better to carry out the prevention of a disease, preventing its development, than to deal with it or its consequences later. To prevent uterine varicose veins, follow these simple guidelines:
- lead a mobile lifestyle, walk more and walk;
- do gymnastic sports;
- eat healthy food, less fatty, fried, spicy, spicy, sour;
- visit the gynecologist regularly, especially at the slightest complaint.

Despite the difficulties in detecting varicose veins of the uterine veins, in order to avoid the progression of the disease and complications, if the symptoms described earlier appear, consult a doctor. It is also important to remember that self-treatment in such cases is contraindicated, careful diagnosis and constant monitoring by a gynecologist and phlebologist are necessary.












































